In the realm of medical breakthroughs, the Human Papillomavirus (HPV) vaccine has long been hailed as a triumph against a variety of cancers, most notably cervical cancer. However, amidst its celebrated conquests, a lesser-known victory quietly unfolds: the HPV vaccine’s unexpected effectiveness against plantar warts. While plantar warts might seem like a minor inconvenience compared to the grave threat of cancer, they can inflict considerable pain and discomfort on those affected. This article delves into the intriguing connection between the HPV vaccine and plantar warts, shedding light on the science behind this unexpected benefit and exploring the potential impact it could have on both the field of dermatology and the lives of individuals plagued by these stubborn growths. Join us as we uncover the hidden dimensions of the HPV vaccine’s influence, transcending its primary purpose to offer relief to those who suffer from an all-too-familiar annoyance: plantar warts.
Comprehensive Guide to Plantar Warts: Causes, Diagnosis, and Distinctions
Origins and Impacts of Plantar Warts
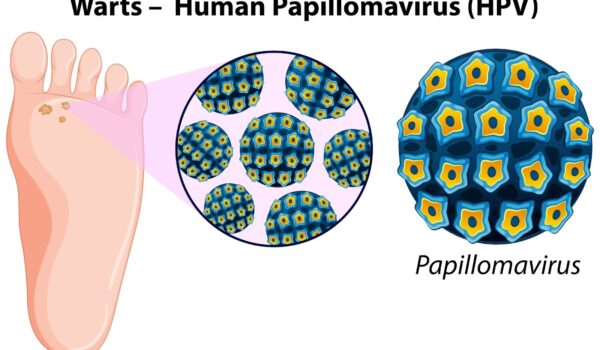
Plantar warts stem from an infection with the human papillomavirus (HPV), a widespread virus with various strains, each leading to distinct clinical manifestations. The primary culprits behind plantar warts include HPV strains 1, 4, 27, and 57.
Insights into the Prevalence:
- Although accurate and comprehensive epidemiological data on plantar warts is scarce, these warts predominantly afflict children and adolescents;
- Despite being benign in the majority of cases, these warts shouldn’t be trivialized. Besides being physically uncomfortable, they often lead to emotional distress and self-consciousness due to their appearance;
- Pain is a common symptom, particularly when these warts are located in areas of the foot bearing weight or if they chafe against shoes;
- In exceptional situations, especially among immunocompromised individuals, these warts can evolve into severe conditions like squamous cell carcinoma or plantar verrucous carcinoma.
Diagnosis and Key Distinguishing Features
The identification of plantar warts is largely reliant on their clinical presentation.
Features of Plantar Warts:
- Skin Thickening: One of the hallmarks of warts is hyperkeratosis, which results in skin thickening;
- Location: They predominantly emerge on foot areas that endure pressure;
- Internal Markings: Tiny specks or streaks, ranging from reddish to brown shades, are often visible within the wart. These are broken capillaries.
Enhanced Diagnosis with Dermatoscopy:
- Professionals with training can employ a dermatoscope, a specialized tool, to enhance the diagnostic accuracy;
- Using a dermatoscope, the broken capillaries appear as red or purple dots, encircled by white rings which are keratin structures;
- Revealing the underlying blood vessels can be achieved by gently removing the outer hyperkeratotic layers.
Distinguishing from Corns and Calluses:
- Corns: Identified by a translucent core. Dermatoscopy highlights concentric fine white rings;
- Calluses: Exhibit a diffused opacity across the lesion, appearing structureless under a dermatoscope;
- Mosaic Warts: An intriguing development is when multiple neighboring verrucae amalgamate to create what’s termed as ‘mosaic warts.’
Points of Caution:
- Although instances are rare, it’s crucial to rule out melanoma when diagnosing a plantar wart;
- Additionally, other tumors can occasionally manifest in similar regions.
Recommendations for the General Public:
- Always consult a medical professional if suspicious foot lesions appear;
- Consider dermatoscopy for a clearer diagnosis, especially in ambiguous cases;
- Prioritize foot hygiene and care, as this can deter the development of plantar warts;
- Remain vigilant and informed about the differences between warts, corns, and calluses. Knowledge can mitigate unnecessary stress and enable timely medical intervention.
HPV Vaccine: What it Covers
The primary goal of HPV vaccines, such as Gardasil 9, is to prevent cancers and other conditions caused by HPV. These vaccines provide immunity against multiple strains of HPV, including those most commonly linked to cancers and genital warts.
It’s crucial to note that while these vaccines target several HPV strains, they do not specifically focus on the strains causing plantar warts. However, there is incidental evidence suggesting some reduction in the prevalence of non-genital warts following vaccination, though this is not the primary intention of the vaccine.

A Comprehensive Guide to Treating Recalcitrant Warts: Spotlight on HPV Vaccine & More
Warts, small and often unsightly skin growths, are typically caused by the human papillomavirus (HPV). While a plethora of treatment options exist, stubborn warts, or recalcitrant warts, have always puzzled even the most seasoned clinicians.
Breakthroughs with Intralesional HPV Vaccine
In recent years, there has been an emerging trend to use intralesional HPV vaccines, especially in cases where conventional treatments have failed. A retrospective study in 2019 by Waldman et al. reviewed 16 cases of stubborn warts treated with an intralesional quadrivalent HPV vaccine:
Key Findings:
- A success rate of 44.0% was observed, with 7 patients experiencing complete wart clearance;
- These results were in line with outcomes from other treatments like Candida antigen, imiquimod, and squaric acid dibutylester.
A more recent study delved into the potential of the intralesional 9-valent HPV vaccine:
Study Design:
- An open-label, uncontrolled, single-arm approach;
- Focused on 45 patients primarily having plantar/periungual warts;
- The vaccine was administered at intervals of 0, 2, and 6 months. The patients’ conditions were reviewed three months post the last injection.
Results:
- A noteworthy clearance rate of 62.2%, translating to 28 patients;
- No wart reoccurrence noted during the observation period;
- A differential response was seen based on age. Patients between 9-26 years had a higher response rate (84.0%) compared to those above 26 years (55.0%).
Insights:
- HPV vaccine, notably the 9-valent type, is shaping up as a promising tool against recalcitrant warts;
- The vaccine offers benefits such as minimized pain and increased convenience when juxtaposed with traditional methods;
- While there’s a pressing need for controlled studies for a definitive verdict on its efficacy, the intralesional 9-valent HPV vaccine is an avenue worth exploring for clinicians.
There’s an added advantage for candidates below 46 years who are eligible for HPV vaccination – not only can it treat stubborn warts, but it also offers protection against HPV-related anogenital cancer.
Exploring Beyond HPV Vaccines: Potential Intralesional Treatments
The medical community is in relentless pursuit of alternative intralesional treatments for stubborn warts. Some agents, in their nascent research stages, have shown significant potential:
- Vitamin D: Emerging as a potential game-changer, with studies hinting at its role in skin health and immune modulation;
- Zinc: Known for its immune-enhancing properties, making it a contender in wart therapy;
- Bleomycin: Traditionally used in chemotherapy, it’s showing promise in the dermatological arena;
- Cidofovir: An antiviral agent, its role in tackling warts caused by viruses is under exploration.
The path to defeating recalcitrant warts is paved with innovative approaches, and the HPV vaccine, especially the 9-valent variant, appears to be a frontrunner. Coupled with other budding intralesional treatments, the future seems bright for those grappling with persistent warts. Always consult with healthcare professionals for personalized advice and treatment options.
Conclusion
While the primary goal of the HPV vaccine is to protect against high-risk strains linked to cancers and genital warts, it’s important to remain aware of and practice preventive measures against other strains, like those causing plantar warts. Understanding the broader scope of HPV and its manifestations helps ensure better health outcomes for all. Always consult with healthcare professionals regarding HPV-related concerns or treatments.