Diphtheria, an acute bacterial illness, is caused by toxin-producing strains of Corynebacterium diphtheriae. Its name finds its origin in the Greek word “diphthera,” which translates to ‘leather hide.’ This disease’s historical roots trace back to the 5th century BCE when Hippocrates documented it, with further descriptions of epidemics provided by Aetius in the 6th century AD. The bacterium itself came under scientific scrutiny when Edwin Klebs first observed it within diphtheritic membranes in 1883, later cultivated by Friedrich Löffler in 1884. Early attempts at prevention in the early 1900s involved combining toxin and antitoxin. However, it wasn’t until the early 1920s that the diphtheria toxoid was developed, though widespread usage only began in the early 1930s. Subsequently, it was integrated with tetanus toxoid and pertussis vaccine, eventually becoming a standard immunization practice in the 1940s.
The Origins of the Name “Diphtheria”
- Hippocrates documented it in the 5th century BCE;
- Epidemics were recorded in the 6th century;
- The bacterium was initially observed in 1883 and later cultivated in 1884;
- The development of the Diphtheria toxoid occurred in the 1920s.
Diphtheria, previously known by various names, acquired its official designation from the French physician Pierre Bretonneau (1778-1862), who coined the term “diphtérite.” The term originates from the Greek word for “leather” or “hide,” which aptly describes the characteristic throat coating known as the pseudomembrane. Bretonneau’s work also involved distinguishing diphtheria from scarlet fever.
Bretonneau notably documented the initial successful implementation of tracheotomy in a case of diphtheria. This surgical procedure, employed for other medical conditions as well, entails creating an incision in the trachea and introducing a tube through the opening to facilitate air passage and secretion removal. While Bretonneau had previously attempted the procedure with unfortunate outcomes, another French physician, Armand Trousseau (1801-1867), later demonstrated a remarkable 25% survival rate in the tracheotomies he conducted on individuals afflicted by diphtheria.
Understanding the Pathogenesis of Diphtheria
The pathogenesis of diphtheria revolves around the acquisition of toxigenic diphtheria bacilli in the nasopharynx by susceptible individuals. These bacteria produce a potent toxin that disrupts cellular protein synthesis, leading to local tissue damage and the formation of the characteristic pseudomembrane associated with this disease.
The toxin, generated at the site of the pseudomembrane, is absorbed into the bloodstream and subsequently distributed throughout the body’s tissues. This toxin plays a pivotal role in causing major complications, including myocarditis, polyneuropathies, nephritis, and even thrombocytopenia.
Non-toxin-producing strains of C. diphtheriae can also lead to illness, ranging from mild to severe exudative pharyngitis. Although rare, severe cases with pseudomembranes caused by such strains have been reported. It’s possible that these infections were triggered by undetected toxigenic strains due to inadequate culture sampling. Additionally, nontoxigenic C. diphtheriae infections can manifest as cutaneous lesions, endocarditis, bacteremia, and septic arthritis, further emphasizing the diverse clinical presentations of this bacterium.
Symptoms and Its Culprit
Diphtheria, a menacing ailment, is brought about by the notorious bacterium known as Corynebacterium diphtheriae. This insidious bacterium possesses the ability to release a potent toxin capable of inflicting substantial harm upon the body’s tissues.
In its early stages, diphtheria cunningly disguises itself as a common cold, manifesting symptoms such as a sore throat, loss of appetite, and fever. However, as the disease advances, a distinctive hallmark of diphtheria infection often emerges: the formation of a dense gray substance referred to as a pseudomembrane. This pseudomembrane can extend its insidious grip over the nasal tissues, tonsils, larynx, and/or pharynx.
The pseudomembrane, a sinister byproduct comprised of waste materials and proteins linked to the bacterial toxin, adheres tenaciously to these delicate tissues and may precipitate breathing obstruction, making diphtheria a perilous and potentially deadly disease.
Clinical Aspects of Diphtheria
Diphtheria, a formidable disease, unveils its clinical manifestations with intriguing characteristics. The incubation period typically spans from 2 to 5 days, occasionally ranging from 1 to 10 days. This insidious ailment can infiltrate nearly any mucous membrane within the body.
In individuals left untreated, the diphtheria-causing organisms can persist in discharges and lesions for an extended period, often ranging from 2 to 6 weeks after the initial infection. To facilitate clinical evaluation and management, it proves advantageous to categorize diphtheria based on its anatomical presentation. This classification distinguishes between respiratory manifestations (such as pharyngeal, tonsillar, laryngeal, and nasal involvement) and non-respiratory presentations (including cutaneous and other mucous membrane manifestations). This comprehensive classification allows healthcare professionals to better understand and address the diverse clinical aspects of this ailment.
Diphtheria Transmission
Diphtheria spreads from person to person, typically through respiratory droplets. An infected individual, unless promptly treated with antibiotics, remains contagious for a duration of two to three weeks.
Treatment and Care for Diphtheria
Managing diphtheria necessitates a combination of antibiotics to eradicate the diphtheria bacteria and antitoxin to neutralize the toxins produced by these bacteria. Patients with diphtheria are commonly isolated until they are no longer capable of transmitting the disease, which typically occurs approximately 48 hours after commencing antibiotic treatment.
Diphtheria Complications
- The primary source of complications stems from the toxin;
- The severity of complications tends to parallel the local disease’s extent;
- Myocarditis and neuritis stand out as the most common complications;
- Mortality rates range between 5% and 10%.
Diphtheria’s potent toxin can wreak havoc on various vital organs, including the heart, muscles, kidneys, and liver, potentially causing temporary or permanent damage. Complications associated with diphtheria encompass myocarditis (heart muscle damage), neuritis (nerve inflammation leading to nerve damage, paralysis, respiratory failure, and pneumonia), airway obstruction, and ear infections.
In the past, diphtheria posed a significant threat to children’s health, with the United States witnessing a peak of 206,000 cases in 1921, resulting in 15,520 fatalities (a case-fatality ratio of 7.5%). Case fatality rates varied, with about 20% for those under age five and over age 40, and 5-10% for those aged 5-40 years. During the 1930s, diphtheria ranked as the third leading cause of death among children in England and Wales. Presently, diphtheria is rare in the United States, with no reported cases between 2004 and 2011 and only one provisional case in 2012. In 2019, two cases were reported, marking the latest available data on diphtheria incidence.
Preventive Measures for Diphtheria
Diphtheria disease does not always provide immunity, so it’s essential to take preventive measures, especially for those recovering from diphtheria who may not have been vaccinated adequately.
For individuals in close contact with diphtheria patients, it’s crucial to assess their vaccination history. If their vaccination record is incomplete or unknown, an immediate dose of diphtheria toxoid-containing vaccine is recommended. The vaccination series should then be completed following guidance from the Advisory Committee on Immunization Practices (ACIP). Even if the contact is up-to-date according to ACIP recommendations but the last dose was administered over 5 years ago, a diphtheria toxoid-containing vaccine should be given without delay.
Additionally, close contacts should receive either a single intramuscular dose of benzathine penicillin G or a 7- to 10-day course of oral erythromycin. Benzathine penicillin G is preferred for contacts for whom continuous monitoring for 7 to 10 days is not feasible. Close contacts should be vigilantly observed, and if any signs of illness appear, prompt diphtheria antitoxin treatment should be initiated.
Early Efforts to Develop the Diphtheria Vaccine
Antitoxin and Serum Therapy
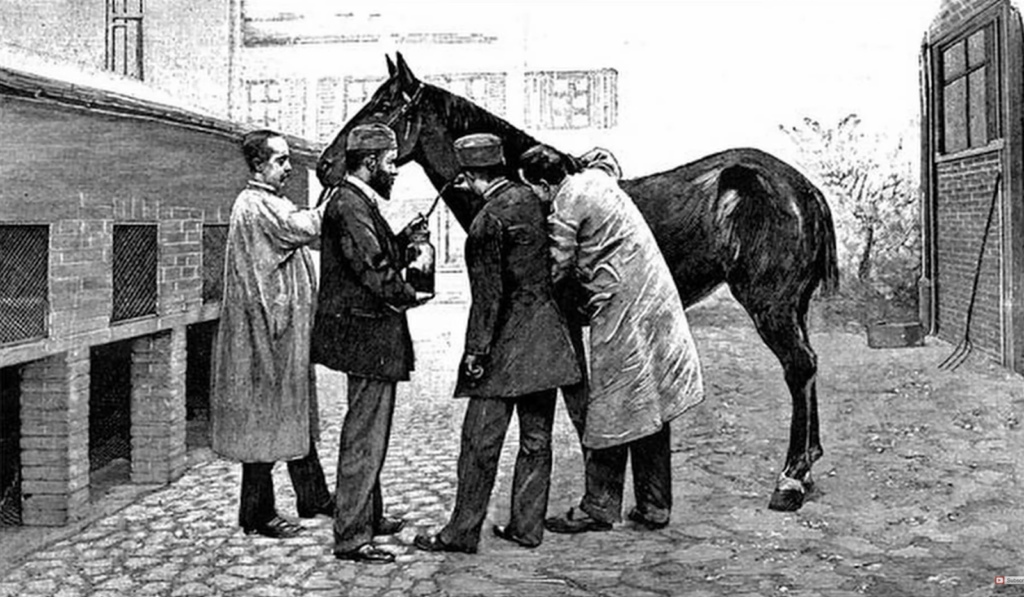
Shibasaburo Kitasato (1852-1931) and Emil von Behring (1854-1917) conducted experiments in which they immunized guinea pigs using heat-treated diphtheria toxin.
Their research revealed that the blood products (sera) of these guinea pigs contained a substance capable of preventing the harmful effects of C. diphtheriae and its toxin when the guinea pigs were subsequently exposed to lethal doses of the bacteria and toxin. They further demonstrated the curative potential of this substance by successfully treating diphtheria in animals through injections of serum from immunized animals. This newfound substance was termed “antitoxin,” and their treatment approach became known as “serum therapy.”
Recognizing the need for larger quantities of antitoxin to safeguard human health, they extended their immunization efforts to larger animals like horses and sheep.
Emil von Behring’s groundbreaking work on diphtheria earned him the distinction of being awarded the inaugural Nobel Prize in Medicine in 1901.
The Tragic Consequences of Antitoxin Contamination
A harrowing episode unfolded as thirteen young lives in St. Louis were tragically claimed by contaminated diphtheria antitoxin.
Upon investigation, it was revealed that one of the horses utilized in the production of diphtheria antitoxin for the St. Louis municipal health authority had succumbed to tetanus. Shockingly, rather than disposing of the tainted antitoxin derived from the deceased horse, some of it found its way into the hands of physicians.
This distressing incident, coupled with a tetanus outbreak in Camden, New Jersey, associated with contaminated smallpox vaccine, prompted the introduction of federal regulations governing biologic products.
Understanding Serum Sickness
Clemens Pirquet (1874-1929) and Bela Schick (1877-1967) made a significant contribution by describing a clinical condition they termed “serum sickness.” This newfound understanding played a pivotal role in shaping our comprehension of allergies and immunological diseases.
Their observations revealed that children treated for diphtheria with substantial amounts of antitoxin derived from horses, sometimes as much as 200 mL (equivalent to nearly 7 ounces or almost 1 cup), often developed symptoms like swelling, fever, rashes, and joint discomfort. It is now understood that the human immune system misidentifies the foreign antibodies present in the serum as antigens, triggering a complex immune response that leads to serum sickness symptoms. Importantly, in Pirquet and Schick’s clinical practice, serum sickness did not pose a life-threatening risk, and the children who recovered from diphtheria were unharmed by this treatment approach.
Lederle Produces Antitoxin
Ernst Lederle, a former New York City Health Commissioner, established Lederle Laboratories in New York City with the primary objective of producing diphtheria antitoxin. Subsequently, the laboratory relocated to a farm situated in Pearl River, New York. Eventually, Lederle Laboratories became integrated into Wyeth Laboratories.
A Milestone in Diphtheria Vaccine Development
As our comprehension of the diphtheria bacterium deepened, the development of a vaccine was on the horizon.
Park’s Breakthrough
William H. Park (1863-1939) conducted pioneering research on diphtheria toxin-antitoxin combinations, initially in animals and subsequently in humans, to establish active immunity. Through meticulous adjustments of the proportions of these substances, he successfully struck a delicate balance between conferring enduring immunity and mitigating adverse reactions to the mixture. This methodology remained in use for human immunization until it was eventually supplanted by toxoid immunization.
Park’s Efforts Against Diphtheria
In 1921, the United States faced a devastating diphtheria outbreak, with a staggering 206,000 reported cases and a tragic death toll of 15,520 (equating to a case-fatality ratio of 7.5%). This marked the darkest year for diphtheria in the 20th century within the nation.
During this crisis, William H. Park initiated a monumental program in New York City. His endeavor aimed to Schick-test schoolchildren and provide immunization to those who had not been exposed to diphtheria through a diphtheria toxin-antitoxin mixture (TAT).
Park’s groundbreaking work in public health required not only the collaboration of numerous school administrators and nurses but also the consent of parents to immunize their children with TAT. An impressive total of 180,000 children were enlisted in this campaign. Half of them were not tested for diphtheria immunity and did not receive TAT. The other half underwent Schick testing, and those testing positive (indicating no prior exposure to diphtheria) received two or three TAT injections to establish immunity.
Over the span of five months, the 90,000 untested children experienced four times as many diphtheria cases compared to the tested and immunized group.
Park’s dedication extended beyond schoolchildren; he sought to extend the benefits of Schick testing and TAT immunization to younger siblings, who faced the greatest risk of contracting and succumbing to diphtheria. Utilizing the school campaign as a platform, he informed parents about immunization opportunities for their infants. This outreach effort included mailing cards, such as the one depicted, which were sent to 45,000 households in New York City, with Italian and Yiddish versions also made available.
Metropolitan Life’s Diphtheria Eradication Initiative
The insurance giant, Metropolitan Life, spearheaded a diphtheria eradication campaign in New York, generously contributing $15,000 to support the cause.
Louis Dublin, a statistician at Met Life, conducted an insightful analysis, estimating that childhood illnesses, including diphtheria, imposed an annual economic burden of approximately $200,000,000 on the American economy, accounting for lost parental wages and medical expenses.
Metropolitan Life employed a multifaceted approach to disseminate the immunization message, utilizing techniques such as door-to-door surveys, radio and print advertisements, essay competitions, parades, and various other outreach methods.
The Proliferation of Outbreaks Amidst War
Amidst the turmoil and upheaval of war in Europe, diphtheria outbreaks emerged as a grave concern. In the year 1943 alone, the continent witnessed a staggering one million cases of diphtheria, resulting in 50,000 fatalities (excluding the USSR).
Transformations in Adult Immunization Practices
The diphtheria toxoid concentration in the adult tetanus-diphtheria booster underwent a reduction.
This adjustment in toxoid concentration resulted in a decrease in adverse reactions, encompassing symptoms like fever, swelling, muscle aches, fatigue, headaches, and chills.
Geoffrey Edsall, a distinguished researcher, provided insights into the reactions associated with the initial booster:
“In adults, reactions to toxoid can be surprisingly severe….[A]n adult [could be] confined to bed for 3 or 4 days, with a massively swollen arm which takes 10 days to 2 weeks to return to normal–all from a standard dose of toxoid…”
–G. Edsall, Immunization of Adults Against Diphtheria and Tetanus, 1954
Advancements in the Diphtheria Vaccine
In various countries, the control of diphtheria, tetanus, and pertussis has been effectively achieved through the utilization of modern vaccine formulations.
The World Health Organization took a significant step by incorporating DTP (Diphtheria, Tetanus, and Pertussis) into its roster of recommended vaccines for the novel Expanded Programme on Immunization designed for developing nations.
By 1974, numerous developed countries had witnessed a remarkable decline in childhood diseases. Nonetheless, these ailments continued to claim numerous lives in less affluent regions. In fact, during 1974, less than 5% of children worldwide received immunization against diphtheria, polio, tuberculosis, pertussis, measles, and tetanus by the age of one. The Expanded Programme on Immunization was established to extend vaccination coverage for these six diseases to numerous underserved regions, marking a pivotal advancement in global healthcare.

WHO’s Endorsement of DTP Vaccination
The World Health Organization incorporated DTP (Diphtheria, Tetanus, and Pertussis) into its list of recommended vaccines for the novel Expanded Programme on Immunization designed specifically for developing nations.
By 1974, numerous developed countries had made significant progress in eradicating childhood diseases. However, these diseases persisted in claiming numerous lives in less privileged regions. Astonishingly, in 1974, fewer than 5% of children worldwide had received immunization against diphtheria, polio, tuberculosis, pertussis, measles, and tetanus by the age of one. The establishment of the Expanded Programme on Immunization marked a transformative initiative aimed at extending vaccination coverage for these six diseases to underserved areas worldwide.
Diphtheria Epidemic in the Russian Federation
Dwindling diphtheria immunization rates in children and diminishing adult immunity contributed to a widespread epidemic in the former Soviet Union. By 1994, the Russian Federation reported a staggering 39,703 cases of diphtheria, a stark contrast to the mere 1,211 cases recorded in 1990.
Diphtheria Eradication in the U.S.: Five Years Without a Case
Respiratory diphtheria has become a rarity in the United States. Remarkably, since 2004, the CDC has not documented any cases of respiratory diphtheria within the country.
In a span of less than 75 years, diphtheria, once the primary cause of premature child mortality, has been effectively eradicated from the United States.
Diphtheria Vaccines and Global Vaccination Efforts
Immunization against diphtheria is achieved through the use of a toxoid, a modified form of the diphtheria toxin. Rather than being administered as a standalone injection, the diphtheria toxoid is typically combined with tetanus toxoid and often the pertussis vaccine, forming preparations known as Tdap, DTaP, Td, or DT.
Since the introduction of effective immunization in the 1920s, diphtheria incidence has seen a substantial decline in the United States and in nations where widespread vaccination practices are adopted. In 1974, the global reach of diphtheria immunization expanded significantly when the World Health Organization incorporated diphtheria toxoid into its recommended immunization list for the Expanded Programme on Immunization, aimed at developing countries.
Between 2004 and 2008, the United States reported zero cases of diphtheria. Nonetheless, the disease continues to be a global concern. In 2007, a total of 4,190 diphtheria cases were documented worldwide, though this figure is likely an underestimate of the actual number of cases occurring globally.
Diphtheria Vaccination Guidelines in the United States
The current U.S. childhood immunization schedule for diphtheria involves administering five diphtheria toxoid vaccinations before a child reaches six years of age, along with an additional booster dose during adolescence. These childhood diphtheria immunizations are administered through injections combined with tetanus toxoid and pertussis vaccine, commonly referred to as DTaP.
For adults, diphtheria toxoid is provided in conjunction with a tetanus toxoid booster, which is recommended every ten years. The adult vaccine can offer protection against both tetanus and diphtheria (referred to as Td) or tetanus, diphtheria, and pertussis (known as Tdap).
Conclusion
The history of the diphtheria vaccine is a testament to the relentless pursuit of medical progress. From its ancient roots described by Hippocrates to the groundbreaking work of pioneers like Pierre Bretonneau and William H. Park, the journey towards comprehensive immunization against this deadly disease has been marked by dedication and innovation. The development of diphtheria toxoid and its integration into routine vaccination in the mid-20th century marked a turning point in public health. Today, thanks to global vaccination efforts and effective immunization schedules, diphtheria has become a rare occurrence in many parts of the world. While we celebrate this achievement, it serves as a reminder of the vital importance of vaccines and ongoing vigilance in the face of infectious diseases.